According to many experts, chronic prostatitis is an inflammatory disease caused by infection with the possibility of exacerbation of autoimmune disorders, characterized by damage to the parenchymal and interstitial tissues of organs. The disease has been known medically since 1850, but to this day the disease is still poorly understood and less responsive to treatment. Chronic bacterial (6-10%) and non-bacterial (80-90%) prostatitis is the most common and significant inflammatory disease in men, which significantly reduces their quality of life. The disease is recorded mainly in young and middle -aged people and is often complicated by disorders of copulator and generative function (decreased potency, infertility, etc. ). The disease is noted in men in 8 - 35% of cases aged between 20 to 40 years.
The cause of bacterial prostatitis is a pyogenic flora, which penetrates into the glands from the urethra, or through lymphogenic and hematogenous pathways. The etiology of chronic non -bacterial prostatitis and its pathogenesis are still unknown. It mainly affects men over 50 years of age.
The causes of the development of this disease
Chronic prostatitis is currently considered a polyetiological disease. There is an opinion that the disease arises as a result of the penetration of infection into the prostate, and then the pathological process runs without its participation. A number of non -infectious factors contribute to this.
Infectious factors in the development of chronic prostatitis
In 90% of cases, the pathogen enters the gland from the urethra, resulting in acute or chronic prostatitis. There have been cases of asymptomatic transport. The course of the disease is influenced by the state of the human body's defenses and the biological nature of the pathogen. It is assumed that the transition from acute to chronic prostatitis occurs due to loss of tissue elasticity due to excessive production of fibrous tissue.
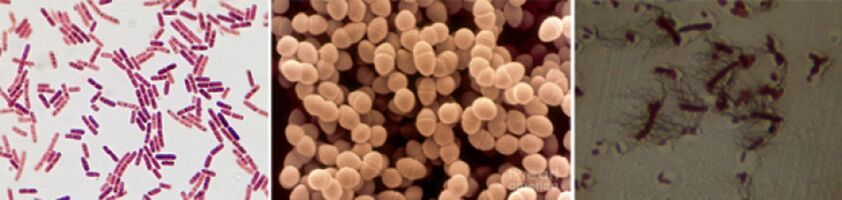
Among the causative agents of chronic prostatitis, the following pathogens have been found:
- In 90% of cases, the disease shows gram -negative bacteria such as Escherichia coli (E. coli), Enterococcus faecalis (fecal enterococcus), quite rarely - Pseudomonas aeruginosa, Klebsiella spp. , Proteus spp. , Pseudomonas aeruginogenes, and Enterobacterer. . Gram -positive bacteria enterococci, streptococci, and staphylococci are rare.
- The role of coagulase negative staphylococci, ureaplasma, chlamydia, Trichomonas, gardnerella, anaerobic bacteria and fungi of the genus Candida has not been fully elucidated.
The infection enters the prostate in several ways:
- The ascending path is most likely, as evidenced by the combination of frequent prostatitis and urethritis.
- Hematogenous prostatitis develops when the infection penetrates into the glands with the bloodstream, which is observed in chronic tonsillitis, sinusitis, periodontitis, pneumonia, cholecystitis and cholangitis, purulent diseases of the skin, etc.
- By contact, chronic prostatitis develops with urethritis and urethra, when the infection enters the ascending glands with urine flow, with purulent infection of the kidneys, through the canalicular ducts for epipidimitis, deferentitis and funiculitis, during diagnostic and therapeutic urological manipulations (catheterization, urethralization), includingtransurethral.
- Lymphogen infection penetrates the prostate with proctitis, hemorrhoidal vein thrombophlebitis, etc.
Non -infectious factors in the development of chronic prostatitis
Chemical factors
According to experts, the main role in the development of chronic prostatitis belongs to intraprostatic urine reflux, when urine is excreted from the urethra into the glands, which causes disruption of the emptying of the prostate and seminal vesicles.
With this disease, vascular reactions develop, causing edema of organs, neural and humoral regulation of urethral smooth muscle tissue tone is disrupted, alpha activationoneAdrenergic receptors cause the development of dynamic blockages and contribute to the development of new intraprostatic reflux.
The veins contained in the urine, with reflux, cause the development of a "chemical inflammatory reaction".
Hemodynamic disorders
They support chronic inflammation and circulatory disorders in the pelvic and scrotal organs. Congestion develops in people who lead an inactive lifestyle, for example, drivers, office workers, etc. , with obesity, sexual abstinence, sexual dysmetry, frequent hypothermia, mental and physical load. Consumption of spicy and spicy foods, alcohol and smoking, etc. , contribute to the preservation of inflammatory processes.
Another factor
There are many other factors that support chronic prostate inflammation. This includes:
- Hormonal.
- Biochemistry.
- The immune response is impaired.
- Autoimmune mechanisms.
- Infectious and allergic processes.
- Structural features of the prostate gland, causing difficulty in bowel movements.
Often, the causes of the development of chronic prostatitis are unlikely to be known.
Classification of prostatitis
According to a classification proposed in 1995 by the U. S. National Institutes of Health, prostatitis is divided into:
- Acute (category I). Is 5 - 10%.
- Chronic bacteria (category II). Is 6 - 10%.
- Chronic non -bacterial inflammation (category IIIA). Is 80 - 90%.
- Chronic non -bacterial pain syndrome (category IIIB) or chronic pelvic pain syndrome.
- Chronic prostatitis, diagnosed by chance (category IV).
Signs and symptoms of chronic prostatitis
The course of chronic prostatitis is long, but not monotonous. The period of exacerbation is replaced by a period of relative calm, which occurs after complex anti-inflammatory and antibacterial therapy.
The development of chronic bacterial prostatitis is often preceded by bacterial urethritis or gonorrhea, not bacterial - circulatory disorders of the pelvic organs and scrotum (hemorrhoids, varicocella, etc. ), sexual excess.
Patients with chronic prostatitis have many complaints. They saw a doctor for years, but were rarely diagnosed with prostate disease. About a quarter of patients do not present any complaints, or the disease persists with few clinical symptoms.
Complaints of patients with chronic prostatitis can be conditionally divided into several groups.
Urinary disorders associated with narrowing of the urethra:
- Difficulty at the beginning of urination.
- Poor urine flow.
- Intermittent or stopped urination.
- The feeling of incomplete emptying of the bladder.
Symptoms due to nerve endings:
- Frequent urination.
- The urge to urinate is sharp and violent.
- Urinate in small portions.
- Incontinence during urgent urination.
Pain syndrome:
- The intensity and nature of the pain vary.
- Localization of pain: lower abdomen, perineum, rectum, groin and lower back, inner thighs.
Sexual dysfunction:
- Pain in the rectum and urethra during ejaculation.
- Slow erection.
- Loss of orgasm.
- Premature ejaculation, etc.
On the part of the nervous system: neurotic disorders in the form of improving patients' attention to their state of health.
Signs and symptoms of chronic non -bacterial prostatitis
Chronic pelvic pain syndrome in men (CPPS) occurs with symptoms common to chronic prostatitis, but bacteria are not present in the 3rd urinary tract and in prostate secretions. CPPS can be simulated by chronic non -bacterial interstitial cystitis, rectal disease, spastic pelvic floor myalgia syndrome and functional prostate lesions caused by disturbances in the organ’s nerve and hemodynamics.
If neurovegetative function is impaired, atony and glandular delay violations are noted, which is indicated by difficulty closing the urethral lumen quickly and completely. At the same time, urine after urination continues to be excreted for a long time gradually. In such patients, studies show instability and increased excitability, which is indicated by increased sweating and stimulation of cardiac activity, dermographic changes.

Complications of the disease
Chronic prostatitis is complicated by sexual and reproductive dysfunction, the development of diseases such as vesiculitis and epipidymitis, as well as hardening of the organs. Organ sclerosis worsens local microcirculation and urodynamics, as well as the result of surgical intervention. Fibrosis of the periuretic tissue leads to the development of urinary disorders.
Diagnostics
Because there are many reasons for the development of chronic prostatitis, various diagnostic studies are used to diagnose it. The success of treatment depends on determining the correct cause of the disease. The diagnosis of chronic prostatitis is based on the following data:
- The classic symptom triad.
- A set of physical methods (digital rectal examination of the prostate).
- A set of laboratory methods (analysis of urine and microscopy of prostate secretions, culture and determination of the sensitivity of the microflora to antibacterial drugs, general analysis of urine and blood).
- For gonococcal detection, smear bacterioscopy of the urethra, PCR and serological methods (for detection of ureaplasma and chlamydia).
- Urofluometers.
- Prostate biopsy.
- Complex instrumental methods (ultrasound).
- Determination of the patient's immune status.
- Determination of neurological status.
- If treatment is ineffective and complications are suspected, magnetic resonance imaging and blood culture, etc.
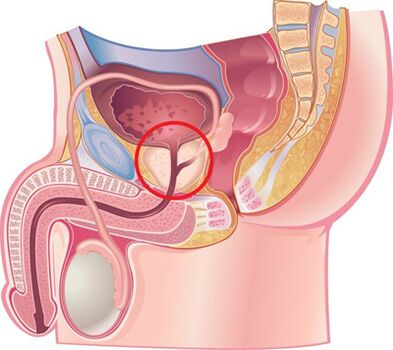
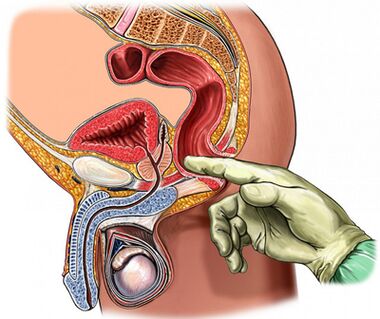
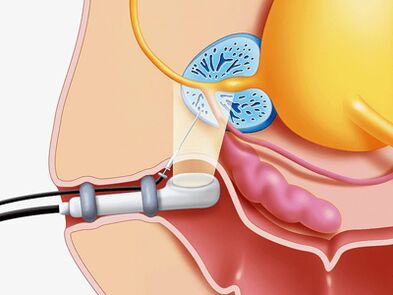
Palpation of the prostate
The most important in the diagnosis of this disease is palpation of the prostate, which increases during the period of exacerbation and decreases during the period of reduction of the inflammatory process. In chronic prostatitis during iron supplementation, it is edematous and painful.
The density of organ consistency can vary: the softening and compaction fields are palpated, the depression zone is determined. On palpation, it is possible to assess the shape of the gland, the condition of the seminal tuberculosis and the surrounding tissue.
The process of transrectal digital examination is combined with the collection of glandular secretions. Sometimes it is necessary to obtain secrets from each section separately.
Analysis of 3 glasses of urine samples and prostate secretions
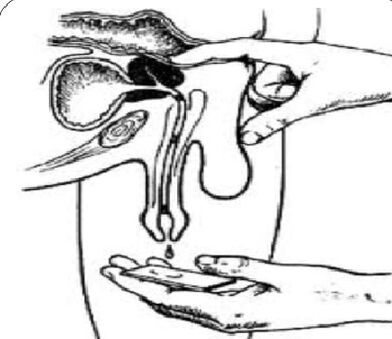
The "gold standard" in the diagnosis of chronic prostatitis is:
- Collection of the first part of urine.
- Collection of the second part of the urine.
- Obtain glandular secretions by massaging.
- Collection of the third part of urine.
Next, microscopic and bacteriological examination of the material was performed.
With inflammation of the prostate:
- Microbial count (CFU) exceeds 103/ ml (10four/ ml for epidermal staphylococci), but do not ignore a small number of microbes in the tens and hundreds.
- The presence of 10–15 leukocytes in the field of view, detected by microscopy, is a generally accepted criterion for the presence of inflammatory processes.
The 3rd prostate and urine secretions undergo microscopic and bacteriological examination:
- In chronic bacterial prostatitis, there is an increase in the number of leukocytes in the glandular secretions and the urine portion of the third post -massage, bacteria (mainly from the intestinal group) are released.
- With non -bacterial prostatitis, there is an increase in the number of leukocytes in the glandular secretions, but the microflora cannot be detected.
- With CPPS, there is no increase in the number of leukocytes and microflora.
Normal level of prostate secretion:
- Leukocytes less than 10 in the field of view.
- There are many lecithin grains.
- Microflora is not present.
In chronic prostatitis, prostate secretions show:
- The number of leukocytes is large - more than 10-15 in the field of view.
- The amount of lecithin seeds is reduced.
- The pH of the secretion shifts to the alkaline side.
- The acid phosphatase content is reduced.
- Increased lysozyme activity.
Obtaining negative results from prostate secretion does not prove in the absence of inflammatory processes.
Prostate secretion crystallization test values were maintained. Usually, during crystallization, a characteristic pattern is formed in the form of fern leaves. In the event of a violation of the aggregation properties of prostate secretions, such a pattern is not formed, which occurs when the background of androgenic hormones changes.
Ultrasound procedure
If prostate disease is suspected, ultrasound examination of the gland itself (transrectal ultrasound is optimal), kidneys and bladder, which makes it possible to determine:
- The volume and size of the glands.
- The presence of calculi.
- The size of the seminal vesicles.
- The condition of the bladder wall.
- The amount of urine residue.
- Scrotal structure.
- Other types of pathology.
Another method of examining the prostate
- Urodynamic conditions (studies of urine flow rate) are determined easily and simply using studies such as uroflowmetry. With the help of this study, it is possible to detect signs of bladder obstruction in a timely manner and perform dynamic observations.
- Puncture biopsy is performed if abscess formation, benign hyperplasia and prostate cancer are suspected.
- To elucidate the causes of the development of infravesicular obstruction, X-ray and endoscopic studies were performed.
- With long -term inflammatory processes, it is recommended to perform urethrocystoscopy.
Differential diagnosis
Chronic prostatitis should be distinguished from vesiculoprostatostasis, autonomic prostatopathy, congestive prostatitis, pelvic floor myalgia, neuropsychiatric disorders, pseudodyssynergy, reflex sympathetic dystrophy, inflammatory diseases of other organs: interstitial cystitis, osteitis of the vesicular articulation, hyperthermia, prostate cancer, prostate, hyperthermiavernicularis, prostate cancer, prostate hyperitis, prostate cancer, prostate hyperitis, prostate cancer, prostate cervitis, prostate cystitis, hyperemia, hypertricularis, urolithiasis prostate cancer, chronic epipidimitis, inguinal hernia.
Treatment of chronic prostatitis
Treatment of chronic prostatitis should begin by changing the lifestyle and diet of the patient.
In the treatment of this disease, drugs are used simultaneously that affect the relationship of different pathogenesis.
The main indications of therapy:
- Elimination of causative microorganisms.
- Anti-inflammatory therapy.
- Normalizes blood circulation in the prostate and pelvic organs.
- Normalization of prostate acini drainage is adequate
- Normalization of the hormone profile.
- Prevention of organ hardening.
For the treatment of chronic prostatitis, the following groups of drugs are used:
- Antibacterial.
- Anticholinergics.
- Vasodilator.
- Alphaone- Adrenergic blockers.
- 5 alpha reductase inhibitors.
- Cytokine inhibitors.
- Non-steroidal anti-inflammatory.
- Angioprotectors.
- Immunomodulator.
- Drugs that affect venous metabolism.
Antibiotics in the treatment of chronic bacterial prostatitis
Antibiotic therapy should be performed taking into account the sensitivity of identified microorganisms to antibiotics. If the pathogen is not identified, empirical antimicrobial treatment is used.
The drugs of choice are generation II-IV fluoroquinolones. They quickly penetrate into the glandular tissue by the usual methods of use, active against a large group of gram-negative microorganisms, as well as ureaplasma and chlamydia. In the event of failure of antimicrobial treatment, one should consider:
- resistance of the microflora of various drugs,
- short course of treatment (less than 4 weeks),
- the wrong choice of antibiotic and its dosage,
- pathogen type changes,
- the presence of bacteria living in the prostate duct, covered with a protective extracellular membrane.
The duration of treatment should be at least 4 weeks with mandatory subsequent bacteriological control. If there are more than 10 bacteria in the 3rd part of urine and prostate secretions3CFU / ml, antibiotic therapy was repeatedly prescribed for a period of 2 to 4 weeks.
Cytokine inhibitors in the treatment of chronic prostatitis
Cytokines are glycoproteins secreted by the immune and other cells in response to inflammatory responses and immune responses. They take an active part in the development of chronic inflammatory processes.
Non-steroidal anti-inflammatory drugs
Non-steroidal anti-inflammatory drugs have anti-inflammatory effects, relieving pain and fever. They are widely used in the treatment of chronic prostatitis in the form of tablets and suppositories. The most effective route is rectal administration.
Immunotherapy
In the treatment of chronic bacterial prostatitis, in addition to antibiotics and anti-inflammatory drugs, immunomodulatory agents are used. The most effective is the rectal route of their administration. Immunomodulators are widely used, which increase the activity of functional phagocytes, which contributes to more effective elimination of pathogens.
Alpha blockers in the treatment of chronic prostatitis
It has been shown that alpha-1 adrenergic blockers normalize the smooth muscle tone of the prostate urethra, seminal vesicles and prostate capsules, which makes drugs of this group very effective in treating this disease. Alpha-1 adrenergic blockers are used in patients with severe urinary disorders in the absence of an active inflammatory process.
With CPPS, the treatment period is 1 to 6 months.
5a-reductase inhibitors in the treatment of abacterial prostatitis and CPPS
It was found that under the influence of the enzyme 5a-reductase, testosterone is converted into the prostate form 5a-dihydrotestosterone, whose activity in prostate cells is more than 5 times higher than the activity of testosterone itself, which in the elderly leads to organ enlargement due to epithelial and stromal components.
While taking 5a -reductase inhibitors for 3 months, stromal tissue atrophy was observed, within 6 months - glands, secretory function was inhibited, the severity of pain syndrome and glandular volume decreased, organ tension and edema decreased.
The role of anti-sclerotic drugs in the treatment of chronic prostatitis
With prolonged inflammation of the prostate gland, fibrosis develops, which is indicated by disturbed microcirculation and urodynamics. To prevent the process of fibrosis, anti-sclerotic drugs are used.
Other medications used to treat chronic prostatitis
Along with the medications mentioned above, the following are used to treat this disease:
- Antihistamines.
- Vasodilators and angioprotectors.
- Immunosuppressant.
- Drugs that affect venous metabolism and trisodium salt of citric acid.
Herbal products
Effective in the treatment of prostatitis is the use of preparations in the form of suppositories containing a complex of biologically active peptides isolated from the bovine prostate gland.
Under the influence of drugs occur:
- Stimulation of metabolic processes in glandular tissue.
- Improves microcirculation.
- Reduction of edema, leukocyte infiltration, secretory stagnation and pain.
- Prevention of thrombosis in the venula of the prostate gland.
- Increased activity of the acini secretory epithelium.
- Improves sexual function (increases libido, restores erectile function and normalizes spermatogenesis).
Massage the fingers of the prostate gland
A number of researchers argue that finger massage should be used for chronic prostatitis, taking into account known contraindications.
Physiotherapy
The effectiveness of physiotherapeutic procedures in the treatment of prostatitis has not been proven today, the mechanism of action has not been scientifically proven, and adverse reactions have not been studied.
Prevention of chronic prostatitis
When starting to prevent the development of chronic prostatitis, you should know:
- The risk of developing this disease increases over the years.
- Representatives of the Negroid race are more vulnerable to disease.
- Family predisposition to the disease is not excluded.
People who have a tendency to develop chronic prostatitis should pay more attention to their health condition.
Disease prevention tips:
- Drink plenty of fluids. Frequent urination encourages the release of microflora from the urethra.
- Prevents diarrhea and constipation.
- Eat a balanced diet. Avoid eating foods high in carbohydrates and saturated fats, which cause weight gain.
- You should limit the use of substances that irritate the urethra as much as possible: spicy and spicy foods, smoked meats, sauces and condiments, coffee and alcohol.
- Stop smoking. Nicotine adversely affects the condition of the vascular wall.
- Don't be too cold.
- Do not withhold bladder emptying.
- Follow an active lifestyle, exercise. Exercises to strengthen the pelvic floor muscles, which can relieve venous congestion, which in turn supports normal prostate function.
- Have a regular sex life. Avoid prolonged abstinence. The glands must be immediately freed from the secretion.
- Remain in a monogamous relationship. Sex without hair loss increases the chances of getting a sexually transmitted disease.
- If you have a complaint from the genitourinary organs, contact your urologist immediately.

























